LINKS WE LIKE #37
Health care is one sector for which the massive amount of data produced daily holds great promise. Data from electronic health records, medical devices and health-related apps (and other sources) has grown so large that they exceed human capabilities for analysis. This is where Artificial Intelligence (AI) comes into play. Through various modeling techniques, AI can help medical researchers analyze massive data sets and identify patterns, which can in turn improve medical diagnostic capabilities and health care services. AI is already being applied to improve and accelerate the accuracy of diagnosis and disease screening, develop new medications, and support public health interventions. Numerous research studies focused on AI have helped to identify diseases such as skin cancers, signs of stroke, diabetes complications or eye disease. There have also been initiatives to predict a patient’s response to a treatment, including heart transplant rejection, cancer treatments, and how well immunotherapy will work on patients with melanoma. Besides AI models for treatment prediction and medical diagnosis, there have also been initiatives to develop tools that can increase quality of life for those living with chronic diseases. For example, Project Euphonia is an initiative that focuses on training speech recognition models to aid those suffering from atypical speech patterns caused by certain conditions. Through their work, they have been able to help many people who lost their speaking ability communicate with their family and friends; as in the case of American professional football player Tim Shaw, who progressively lost his speaking ability due to ALS.
The Risks of AI
Despite its great promise, there are many risks that must be considered when using AI for healthcare. One of the biggest risks is replicating human bias through AI models. The Alan Turing Institute identified this situation as one of the biggest obstacles to why, in the United Kingdom, AI had made little impact in fighting the COVID-19 pandemic. MIT Assistant Professor Dr. Marzyeh Ghassem also identified this risk while conducting her dissertation in computer science, when she discovered that models performed differently for certain racial minority groups. Based on this experience she concluded that algorithms developed for care delivery need to be trained with data sets that represent diverse patient populations and not designed using “black box” models. In other words, to avoid replicating these biases, AI research needs to include large, representative, and balanced data sets which have undergone testing to verify their accuracy before being used on actual patients. On this note, Dr.Andrew Ng also highlights another risk, which is that some models use data based on specific training sets that depend on local data, thus their performance may diminish significantly when/if applied in a different context.
How to Overcome These Obstacles?
Although these risks are not issues exclusive to AI’s application in healthcare, it is important to design mitigation and good practice strategies to help practitioners and researchers address them. The WHO, for instance, presented a recent global report on Artificial Intelligence (AI) in health that maps the sector’s progress, obstacles, and future, and outlines six guiding principles for AI’s design and use in health. In terms of research, the AIDE Project, an initiative that seeks to understand the human factors that will help or hinder the implementation of AI in healthcare, has also taken on the task of identifying how AI is expected to impact the healthcare sector and determine the main concerns that need to be addressed to promote its acceptance and adoption. There are also initiatives such as the nonprofit Nightingale Open Science, that are actively working to improve the quality and scale of data sets available to researchers by collecting patient’s data, anonymizing them, and granting access for nonprofit research.
Join us in this edition of Links We Like as we explore some of the ways AI is being used in the healthcare sector, from maternal healthcare to mental health. Resources are available in English, Spanish, and Portuguese.

Emilia Molimpakis, a postdoctoral neuroscience researcher at University College London, felt disillusioned with traditional mental health care after it let down a friend of hers. Rather than complain, however, she did something about it. Recognizing the limitations faced by providers, which have only been exacerbated by the mental health care crisis stemming from the pandemic, Emilia co-founded Thymia. The tool is a simple set of AI-enhanced mobile video games, which the company claims can identify depression as well as an office examination. Co-founder Stefano Goria says this is accomplished by applying mathematical tools to extract information about the user, potentially working better than traditional self-assessments. While playing the simple games, the AI is recording a variety of reactions, which are then processed with an algorithm programmed to identify various mental health conditions. This interesting article explores the current (dire) state of mental health care and some ways that innovators are applying technology to meet these challenges. This includes new technologies, companies and applications, and even some unexpected uses for older tech, such as video games!
Aimentia Health, una empresa emergente impulsada por la Universitat Oberta de Catalunya, usa la inteligencia artificial para recoger datos de pacientes y crear un sistema que genere hipótesis sobre el problema y sus posibles soluciones. Esta plataforma se puso a disposición del personal sanitario en España con el fin de proporcionar apoyo psicológico gratuito las 24 horas del día. En cuanto a los síntomas emergentes de salud mental, Aimentia ha sido capaz de integrarlos en su flujo de inteligencia artificial. Gracias a ello, la herramienta ya puede ofrecer sugerencias de diagnóstico primario, comparando los datos de un paciente con otros registros anónimos y detectando así posibles factores de riesgo De acuerdo con el creador, Edgar Jorba, lo que ha creado su equipo es un lenguaje de programación basado tanto en los síntomas como en los patrones no clínicos que hace comparaciones anónimas entre perfiles, lanza sugerencias sobre posibles diagnósticos o tratamientos, y permite personalizar terapias. La plataforma se describe como un “asistente virtual” para profesionales de la psicología, la psiquiatría y la neurología.
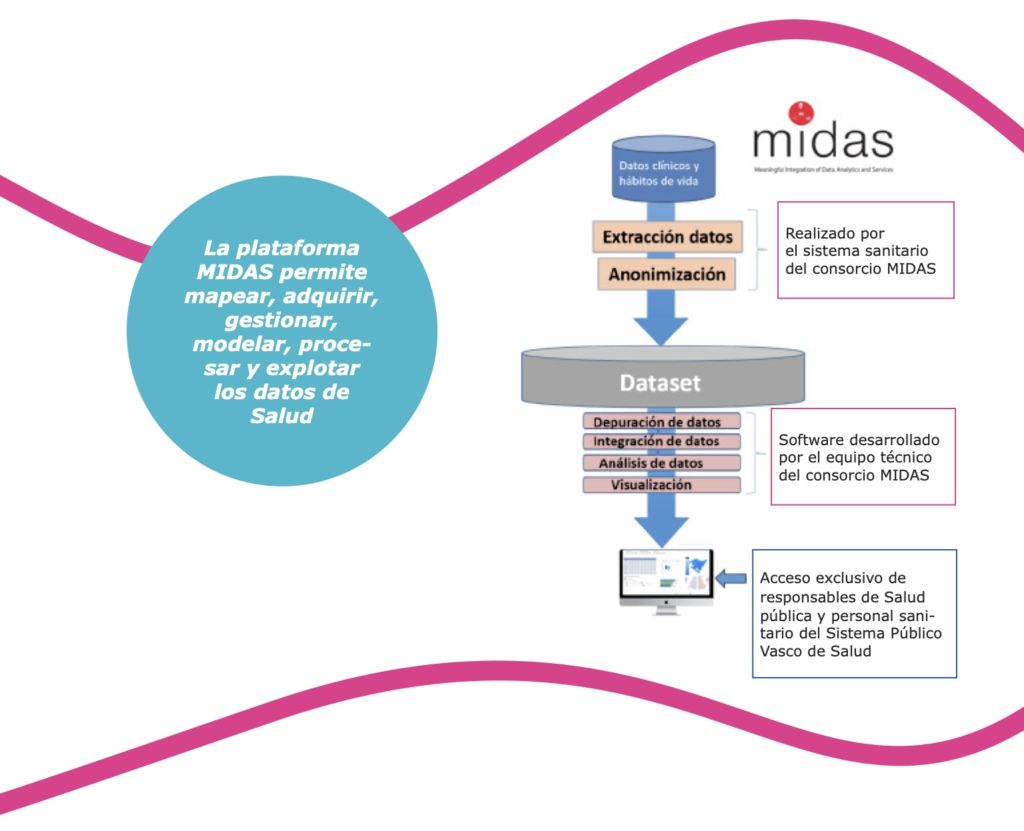
El proyecto MIDAS es un proyecto creado en 2016 con el fin de utilizar el big data para la salud pública. MIDAS significa Meaningful Integration of Data, Analytics, and Services o “Integración Significative de Datos, Analítica y Servicios”. El proyecto está compuesto por cuatro socios: la República de Irlanda, Irlanda del Norte, Finlandia y Euskadi. Gracias a la financiación de la Unión Europea, cada socio investiga un tema en concreto haciendo uso de herramientas para el análisis del big data. La República de Irlanda busca adentrarse en el estudio de la diabetes haciendo un estudio de la distribución de recursos para la lucha contra esta pandemia. Irlanda del Norte investiga la desprotección infantil y las circunstancias que pueden llevar a que niños y jóvenes pasen a estar bajo la protección del estado (y por ende entrar o salir del amparo de los servicios sociales). Finlandia estudia la salud mental y el uso de estupefacientes en jóvenes, explorando cómo se pueden aumentar las fuentes de información para las políticas de prevención. Por último, Euskadi investiga la obesidad infantil y pretende entender sus orígenes para promover intervenciones eficientes. Así, al hacer uso de herramientas del big data, el proyecto MIDAS está teniendo un impacto importante en comunidades y resalta la relevancia de estas nuevas tecnologías –y grandes cantidades de datos– para la salud pública.
Artificial Intelligence (AI) is improving health care delivery systems by making medical technologies for maternal and fetal medicine accessible and affordable. With the use of Al and clinical data, medical complications and defects are diagnosed as early as possible to inform medical decisions. Whereas studies have found a link between Al and predictive medicine, their usage helps in forecasting diseases and other birth defects. Women who experienced complications during delivery or are unable to keep track of menstrual cycles and other vitals are able to deliver more safely and without disorder or defect. In the USA, AI is being used for menstruation tracking. It also provides actionable and real-time tips on how to improve the health of their unborn child. Al has also been increasingly used for ultrasounds, as it speeds up the process. Additionally, it improves fetal surveillance by enabling doctors and practitioners to spot, check and align fetus development with normal anatomy. Whereas embryo selection in the past has been based on morphology (appearance), the degree of accuracy is relatively low (20-35%), thereby reducing the success rate. With the use of Al, doctors can select high-quality embryos for in-vitro fertilization with 97% accuracy, enabling women to have healthier babies.
Iniciativas de acompanhamento e informação por meio de tecnologias digitais têm sido desenvolvidas como alternativas inovadoras para a atenção e cuidado de pacientes em um mundo cada vez mais digitalizado. O aplicativo “Eu Cuido” coleta informações e faz recomendações de ações preventivas personalizadas aos pacientes após uma primeira consulta com um clínico geral, onde dados como o histórico familiar e costumes diários são coletados. Estes dados permitem a análise de possíveis doenças e complicações de saúde a serem enfrentadas pelo paciente, sendo assim, os médicos conseguem informar alternativas e cuidados para impedir e reverter estes possíveis cenários. Por meio do aplicativo, os pacientes também podem acessar informações coletadas durante internações e consultas, como resultados de exames e os medicamentos administrados durante internações. Os desenvolvedores do “Eu Cuido” garantem que o sistema é centrado no paciente e conta com o monitoramento ativo da performance de saúde de maneira individual a partir da busca ativa de dados, um método baseado na medicina de evidência.
Further Afield
Big Data and AI in Healthcare
- The AI Health podcast
- AI in Healthcare with Dale Markowitz
- Health & Veritas: AI, Machine Learning, and Medicine
- Big Data en salud: retos y oportunidades
- La importancia del análisis de datos en la medicina predictiva
- Inteligência artificial na medicina: qual impacto para a saúde?
- Big Data e Inteligencia Artificial para optimización del sistema de salud
- Inteligencia artificial para la salud y la asistencia sanitaria en la UE
- Clinical AI Gets the Headlines, but Administrative AI May Be a Better Bet
- Eficência do Uso de Leito e Inteligência Artificial: a Entrega de Valor em Hospitais Filantrópicos.
- Healthcare 4.0
Risks of AI in Health
- The downside of machine learning in health care
- El desafío del big data en los sistemas de salud
- The Truth About AI in Healthcare
- Healthcare Ethics in AI: Can Software Make Ethical Decisions?
Future of AI in Healthcare
- For Patients to Trust Medical AI, They Need to Understand It
- Trust is AI’s Most Critical Contribution to Health Care
- The future of medical AI
- How AI Will Drive The Precision Health Research Revolution Through 2030
- Big Data y salud: la medicina del futuro
- Big data y el sector de la salud: el futuro de la sanidad
- Cómo el ‘big data’ y la IA pueden mejorar la sostenibilidad del sistema sanitario
- How Artificial Intelligence Could Change the Fertility World
- How AI Could Help Doctors Reduce Maternal Mortality
- The potential of artificial intelligence to bring equity in health care
Healing Patients Through AI
- Healed through AI
- Can A.I.-Driven Voice Analysis Help Identify Mental Disorders?
- Aplicaciones del big data en el sector de la salud
- Big data en sanidad en España: la oportunidad de una estrategia nacional
- Cinco proyectos de inteligencia artificial para predecir enfermedades
- Proyectos de inteligencia artificial, gamificación y home delivery, las nuevas tecnologías al servicio de la salud
- AI & cancer: Big data, big gains for medicine
- Artificial Intelligence Enhanced Heart Disease Diagnosis in Ultrasounds
- How Hospitals are Using AI to Save Lives
- How big data can save lives:Transforming medical care with machine learning
- Artificial Intelligence: A New Paradigm in Obstetrics and Gynecology Research and Clinical Practice
- AI technology to boost maternal health
- Why AI for healthcare is critical in Maternal and Child Healthcare
- Valor Saúde Brasil -Plataforma de governança clínica
- The National Institute of Mental Health’s Dr. Joshua Gordon on AI and Psychology [Podcast]

![M002 - Feature Blog Post [WEB]](https://datapopalliance.org/wp-content/uploads/2025/10/M002-Feature-Blog-Post-WEB.png)